
Keratoconus treatment
We propose reliable progress prevention and comfortable vision correction method.
What is keratoconus?
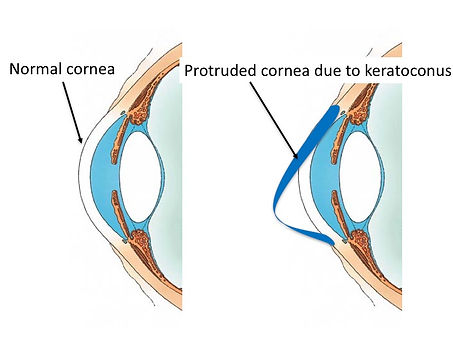
The first place to pass when light enters the eyeball is a transparent place called the cornea, and if you compare the eyeball to a camera, it works as a lens. Because the cornea suffering keratoconus is originally weak, the cornea gradually protrudes towards the anterior side due to the influence of the pressure inside the eye as shown in the figure below. It will protrude and become thinner. As the lens is distorted, various obstacles come up in what you see.
Keratoconus is a disease that often develops in the ten to twenties. When I look at the patient actually coming to my outpatient clinic, they first go to eyeglass shop due to worsening of vision, and since astigmatism is very strong and can not be corrected with eyeglasses, it is often introduced to my clinic so that it is often diagnosed I think.
As the younger a keratoconus is more likely to progress, the uncorrected and corrective vision decrease as the progression progresses gradually, gradually it can not be corrected with eyeglasses. Also, in patients with atopic dermatitis and allergic conjunctivitis and having a habit of rubbing their eyes, the disease is more likely to progress.
Keratoconus is a disease that affects the younger one and affects lifelong visual function. For this reason, early diagnosis and early treatment are important, so I conduct awareness activities through keratoconus study group in Japan and give lectures to general ophthalmologist at ophthalmology conference in Japan.

Treatment to stop the progress of keratoconus, Corneal crosslinking
Corneal crosslinking is the method reported by German ophthalmologist Prof. Seiler in 2003. The cornea is made up of bundles of collagen fiber, and corneal crosslinking is a treatment to increase its strength. The patient's visual acuity is slightly improving by treatment, but because it is basically a treatment for progression prevention, remarkable improvement can not be expected. For this reason, this treatment is mainly targeted at patients in progressive stage, and the main purpose is to prevent disease become worse and avoid cornea transplant.
Surgery is under topical anesthesia (only eye drops), after removing the tissue of the corneal surface, a light-sensitive substance called riboflavin (vitamin B 2) is instilled into the cornea. After that, it irradiates long-wave ultraviolet rays, the cornea reacts with riboflavin, ultraviolet light, and a bridge will be formed between the collagen fibers. This is called crosslinking.
Currently, in Europe and the United States, it is treatment of standard keratoconus but in Japan it is still unauthorized treatment by Ministry of Health, Labor and Welfare, so we are doing it as a self-funded medical treatment after getting approval of ethics committee.
In our facility, we introduced the latest cornea cross linking instrument KXL system manufactured by Avedro Inc., USA, and conducted high speed crosslinking which can shorten the irradiation time of ultraviolet ray, which required 30 minutes of conventional crosslinking, to approximately 10 to 5 minutes.
There are patients who are diagnosed with keratoconus and are worried about suddenly hearing as surgery, but corneal crosslinking is a minimally invasive treatment and is a very safe and reliable treatment.

Contact lens
(RGP and piggyback)
As the keratoconus progresses, you can not correct your eyesight sufficiently with your glasses. In such cases it will be necessary to correct visual acuity with rigid gas permeable contact lenses (RGP). Getting used to RGP from the young age is very important for the future. For this reason, we are focusing on wearing instructions and training in our facilities. We are dealing with several lenses for keratoconus so that we can handle from mild to severe lenses. If it is impossible to fit the RGP lens, we also have a method called piggyback to put a RGP lens on a soft contact lens. When doing this, it often reduces foreign body sensation.
Scleral lens
(Boston scleral lens, PROSE, Miniscleral lens)
Unlike ordinary RGP lens, the characteristic of the scleral lens is that it does not touch the cornea and supports it with the sclera (white part of the eye), which means that there is almost no foreign body feeling. In fact, those who can start this lens are cases where dry eyes are severe and RGP lens can not be worn, when the keratoconus is severe, hard contact lenses can not be worn for a long time.
Since the scleral lens is basically not dropped or shifted, it is also prescribed for those who have difficulty wearing ordinary RGP lenses due to work style etc. It is also suitable for those who do active sports. However, with regard to visual acuity, since it is equivalent to a normal RGP lens, vision may not be improved even with a scleral lens in severe cases. Since this contact lens is an unauthorized treatment by the Ministry of Health, Labor and Welfare, we are prescribing it at the Nagoya Eye Clinic as a self-funded treatment after approval of the ethics committee. I can also prescribe it at Satoh Yuya Eye Clinic in Sendai City.
There are two types of sclera lenses currently handled, Boston lens (PROSE) and Mini Scleral Lens (i-sight scleral). I use it according to the condition of the patient.
Boston scleral lens(PROSE, made at Boston Foundation for Sight, USA):It is a scleral lens that I learned in Boston where I was studying in the past and took it back to Japan. Even among the sclera lens, it is the most historical lens. The characteristic point is that the design can be changed freely so that lens can be prescribed even with very severe keratoconus. Currently Nagoya Eye Clinic prescribes PROSE as a base in Asia and prescribes it to patients from overseas.
Mini scleral lens(i-sight scleral、made at GP specialist, USA):It is a scleral lens which is one size smaller than the Boston lens. Because the diameter of the lens is small, there is the merit that it is easy to wear even those with small eyes. Although we can not change the design freely, it is also beneficial that prices are kept lower than PROSE.

Intracorneal ring surgery
Intracorneal ring surgery is a method of improving the shape of the cornea and correcting corneal distortion by placing a transparent ring in the cornea. It can be applied when RGP lenses can not be worn and you want to improve the uncorrected vision even a little. However, since the corrective effect of the intracorneal ring is inferior to RGP lenses, those with higher severity are not suitable for this purpose.
Another purpose is to improve fitting of RGP lens. In the case of keratoconus cornea, because the cornea is protruding, the same location on the cornea may be scratched with a contact lens and cornea may become opaque. Another purpose is to ease the protrusions of the cornea by corneal ring surgery, making contact lenses easier to ride. Improvement of contact lens fitting can be expected by alleviating corneal protrusion by corneal ring surgery.
At our facility we are conducting corneal ring surgery using a femtosecond laser. By using the femtosecond laser it is possible to safely insert the ring into the cornea at the correct position. Surgery is about 15 minutes.
Combination treatment
Previously, there was only a contact lens in the correction of visual acuity of keratoconus, but by combining several treatments it has become possible for patients with keratoconus to see without glasses and contact lenses, which was not thought before.
Regarding combination therapy, I gave a lecture at the symposium of the Japan Cataract and Refractive Surgery Congress in 2017, and then I published its contents to academic journal.
The main combination treatment is a method of correcting the irregular shape of the cornea with the intracorneal ring and then correcting remaining astigmatism and myopia with a phakic IOL (ICL). In addition, for young people, corneal crosslinking may be done prophylactically so that the surgical effect will not be changed by keratoconus progression in the future.
Cataract surgery for keratoconus
If a keratoconus patient becomes cataract, it can be said that it is a big opportunity in a sense. In other words, it is possible to correct the state where the left and right difference was large or strong astigmatism etc. by the intraocular lens. In some cases it may be possible that patient can see it without using a RGP lens.
However, cataract surgery for keratoconus is difficult in mainly two respects. The first is the error in intraocular lens power calculation. Usually, I will ask patients, how to see after surgery, lifestyle, etc. and adjust the intraocular lens power. However, since the formula is created for the normal one, errors will occur. In order to prevent this, we now use a calculation formula that is designed specifically for keratoconus, or we use a ORA system which can measure and calculate intraocular lens power during surgery to reduce errors as much as possible.
The second difficulty is choosing the type of intraocular lens. In the case of mild keratoconus without postoperative RGP lenses, an intraocular lens with astigmatism correction is a good indication. In the case of moderate to severe keratoconus requiring RGP lenses after surgery, intraocular lenses with astigmatism correction are not applicable. Basically, multifocal intraocular lenses are not applicable when there is an irregular astigmatism like a keratoconus.
Recently, intraocular lenses correcting presbyopia, which can cope with irregular astigmatism such as keratoconus, have been available. IC-8 (AcuFocus) has an pinhole on the intraocular lens, it can reduce the influence of irregular astigmatism and can focus from far to near by pinhole effect. Simulation results compared with single focal intraocular lens (bottom figure), you can see well that the focus is in a wider range than single focal point lens. I am currently using IC-8 at Nagoya Eye Clinic and Chukyo Eye Clinic.


Educational activities on keratoconus
The keratoconus is said to be one to two in 1000 people, it is not a frequent disease. However, I think that its social influence is extremely large, since the onset of disease is from teenagers to twenties and then affects the whole life time.
Previously I could find a keratoconus but could not inhibit progression, and I mainly prescribed contact lenses and corrected visual acuity, and needed to perform corneal transplant if it became severe. At present, keratoconus is early detected and early treated, it is becoming possible to prevent severe status. However, even among ophthalmologists, there are situations where the latest information is not available.
In order to improve this even a little, I am conducting educational activities at the keratoconus study group and conducting lecture activities related to keratoconus in the whole country.

List of lectures
-
JSCRS congress in 2015 (Tokyo)
"Corneal crosslinking, Dresden protocol and accelerated
crosslinking"
-
Gifu Danwakai meeting in 2015 (Gifu)
"Update of keratoconus, from latest diagnosis to treatments"
-
JSCRS congress in 2016 (Kyoto)
"Tips of management after corneal crosslinking, Points of
examinations after reverse referral"
-
Annual congress of Japan clinical ophthalmology in 2017 (Tokyo)
"Other treatments for keratoconus including intracorneal ring and
scleral lens"
-
JSCRS congress in 2017 (Fukuoka)
"Refractive surgery in difficult cases"
-
JSCRS congress in 2017 (Fukuoka)
"Tips of management after corneal crosslinking, Points of
examinations after reverse referral"
-
Keratoconus study group meeting in 2008 (Kyoto)
"Scleral lens prescription for keratoconus"
